
![]()
![]()
![]()
1 Vesna Konjevoda
2 Leonarda Lončar
2 Daniela Raguž
1 Croatian Catholic University, Zagreb, Croatia
2 Clinical Hospital Sveti Duh, Zagreb, Croatia
https://doi.org/10.24141/2/9/2/11
Author for correspondence:
Vesna Konjevoda
Croatian Catholic University, Zagreb, Croatia E-mail: vesna.konjevoda@unicath.hr
![]()
Keywords: patient safety, intrahospital transfer, intrahos- pital transfer protocol, nurses, adverse events
![]()
![]()
![]()
Introduction. The unstructured course of intrahos- pital transfer affects the quality of healthcare. In ad- dition to various clinically unfavorable incidents that prolong hospital stays and indirectly affect positive treatment outcomes, intrahospital transfers lead to
much more complex consequences for the health- care system. Particularly vulnerable and sensitive patients are placed in Intensive Care Units. Nurses have a key role in safe intrahospital transfers.
Aim. This study, based on the available literature, aims to provide a deeper and more comprehensive insight into the incidence of adverse events caused by intrahospital transfer, identify risk factors, deter- mine the need for more extensive surveillance and propose possible solutions for preventing incidents caused by inadequate IHT and improving the quality of healthcare services.
Methods. Review. Search of scientific studies pub- lished from 2019 - 2024 in scientific databases Med- Line and Cochrane.
Results. Research was conducted on 24 studies re- lated to patients and intrahospital transfer. Of the to- tal 24 studies included, 17 focused on adult patients, while the remaining 7 examined healthcare profes- sionals, primarily nurses involved in intrahospital transfer.
Conclusion. Many studies have emphasized the high-quality assessment of the potential benefits of the transfer in comparison with the consequences of adverse events. Special attention has been paid to vitally endangered patients as the most sensi- tive group whose transfers require a multidiscipli- nary approach and a clearly structured course. The implementation of protocols and procedures reduces the incidence of adverse events and deterioration of the patient’s condition during intrahospital transfers. Further studies and meta-analyses are needed.
![]()
![]()
![]()
Numerous studies of different approaches are being conducted to reduce adverse events during intrahospi- tal transfers (IHT). Such studies have been conducted since the 1970s and an increasing number of studies correlate the impact of mistakes in intrahospital trans- fers with a number of factors that contribute to worse clinical outcomes (1). In addition to various clinically unfavorable incidents that prolong hospital stays and indirectly affect positive treatment outcomes, intrahos- pital transfers lead to much more complex consequenc- es for the healthcare system. Besides the individual approach, the impact of complications and deviations from intrahospital transfer guidelines on the hospital as an organizational structure should also be consid- ered. A reliable course of treatment and movement of patients is of great importance for the hospital system. The unstructured course of intrahospital transfers af- fects the patient, but also the health care quality in a wider context (2, 3). Therapeutic and diagnostic pro- cedures, especially for patients who require intensive treatment, are necessary to provide patients with time- ly and appropriate care. Nurses and technicians who supervise the patient during such procedures must possess a wide range of knowledge and competencies to recognize any acute event and react in a timely man- ner with the aim of preventing adverse events or com- plications (4). The studies published so far talk discuss the key role of nurses in ensuring the patient’s safety during IHT (5). Since it is required to have a high level of knowledge and skills that health professionals must master, some studies also suggest the introduction of specialized teams for IHT (6). In order to find an ideal solution, studies have highlighted not only technical challenges but also a significant prevalence of errors stemming from poor judgment, delayed recognition of acute conditions, deviation from established protocols, and gaps in knowledge and skills (7).
Also, as a relatively common cause of adverse events for the patient, studies single out poor communica- tion among health personnel, which results in con- flicts and disobeying the hierarchical structure when making medical decisions (8). The number of intra- hospital transfers during a stay in a healthcare facil- ity is ultimately reflected in psychological alterations in patients, as well as in lower satisfaction with the healthcare services (9).
![]()
This study, based on the available literature, aims to provide a deeper and more comprehensive insight into the incidence of adverse events caused by intra- hospital transfer, identify risk factors, determine the need for more extensive surveillance and propose possible solutions for the purpose of preventing in- cidents caused by inadequate IHT and improving the quality of healthcare services.
![]()
![]()
Available studies published in the last 5 years, from 2019 - 2024, in scientific databases MedLine and Cochrane were searched.
The search keywords were patient safety, intrahospi- tal transfer, nurses.
The search resulted in 674 papers published in the last 5 years. Adding additional keywords such as ‘adverse events’ and ‘intrahospital transfer protocol’, and narrowing the search to a specific goal, resulted in 24 papers, which were then further examined and analyzed according to the stated inclusion criteria.
The basis of the search was to gain insight into the incidence of adverse events caused by intrahospital transfer, identify risk factors, determine the need for more extensive surveillance and propose possi- ble solutions for the purpose of preventing incidents caused by inadequate IHT and improving the quality of healthcare services.
Phase 1 consisted of defining the inclusion and ex- clusion criteria for this review paper.
Phase 2: Reviews of the above scientific databases using the initial keywords resulted in 674 identified studies. Further filtering regarding specific objec- tives and keywords resulted in 17 studies concern- ing adult patient population and 7 studies concern- ing healthcare professionals.
Phase 3: Thorough analysis and reading of studies. Phase 4: Writing the review paper
![]()
![]()
Table 1. Exclusion and inclusion criteria | |
INCLUSION CRITERIA | EXCLUSION CRITERIA |
Papers published in the last five years | Papers published more than five years ago |
Methodologically correctly systematized papers with a clearly defined type of research, goals, methods, and results | Methodologically incorrect and inconsistent research |
Papers presenting intrahospital transfers and their components | Papers addressing exclusively transfers outside the hospital, i.e. from one institution to another |
Cross-sectional studies, retrospective studies, prospective studies, observational studies, cohort studies, review papers | Scientific articles addressing the evaluation of ‘checklists’ and the implementation of newly formed ‘checklists’ at the level of one institution on a statistically insignificant, i.e. insufficient sample |
Scientific papers describing the intrahospital transfer of adult patients related to intensive care medicine, surgery, neurology, diagnostic procedures such as magnetic resonance imaging (MRI) and multi slice computed tomography (MSCT) that require intrahospital transfer and those papers describing the impact of protocol implementation and structured communication on the quality of intrahospital transfers | Scientific papers describing intrahospital transfer in any other context |
Free access to full text | Paywalled papers |
![]()
A total of 17 studies for adults and 7 studies regard- ing healthcare professionals’ perspective were iden- tified and analyzed. The majority of studies were cross-sectional or retrospective. Research was con- ducted on a sample of 56,840 adult patients, one meta-analysis that includes 12,313 within hospital transports and 1,898 patients from 24 studies. A total of 7 of the 24 included studies refer to a sam- ple of 1,395 healthcare professionals, mostly nurses participating in IHT.
![]()
![]()
This review aims to provide insight into the course of IHT, describe the incidence and nature of the most frequent adverse events, bring closer the importance of attention to vitally endangered pa- tients, and demonstrate the importance of integrat- ing protocols and communication structures. The analysis includes studies that, prompted by a large number of incidents, address the flow, the biggest problems, and available tools for improved IHT be- tween various wards. Based on the inclusion and exclusion criteria, the discussion includes 24 stud- ies describing IHT from different perspectives. The study provides an in-depth analysis of the signifi- cance of the structured course to IHT, highlighting its impact on both the patients and the hospital as an organizational structure. Special attention is paid to the most vulnerable groups of patients - unstable and vitally endangered patients. Also, these studies provided an insight into the most common reasons for transfers of such patients within the institution, as well as the most frequent adverse events that occur during such transfers. IHT play a critical role when it comes to improving safety and achieving the best treatment outcomes. Numerous studies have demonstrated progress in this area using vari- ous protocol and communication tools that contrib- ute to the structured course of IHT.
screening:
Figure 1. PRISMA flow diagram
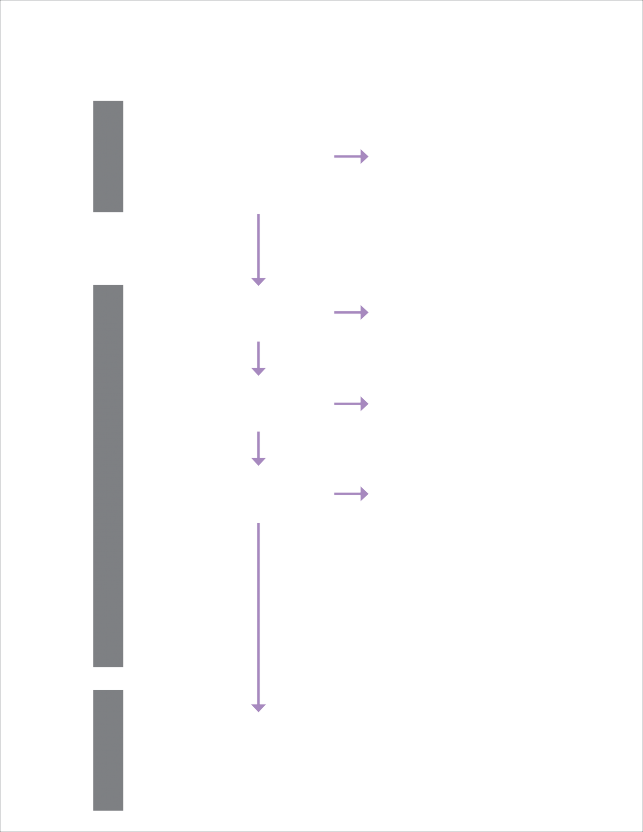
Table 2. Studies included regarding adult patient intrahospital transfer | ||||
Author, year, country of origin | Type of study | Sample and time of research | Research objective | Conclusion |
Ling L, Xia X, Yuan H, et al., 2023. China | Retrospective study | Intensive Care Unit (ICU) patients Control group (n=420) Observational group (n=380) From June to December 2017 and from January to June 2018. | To assess the effectiveness of a graduated model of intrahospital transfer. | Duration of intrahospital transfers and reduction of adverse events are significantly lower, but not related to length of stay and mortality. |
Zirpe KG, Tiwari AM, Kulkarni AP, et al., 2023. India | Observational study | ICU patients (n=893) From March 2022 to February 2023. | To determine the incidence, severity, and effects of adverse events on patients. | High incidence of adverse events, but not associated with mortality. |
Parveez MQ, Yaddanapudi LN, Saini V, et al., 2020. India | Prospective observational study | ICU patients (n=160) 8 months | To determine the incidence and types of adverse events (AEs) during IHT | Most IHTs occur for the purpose of diagnostics and small procedures, procedures that can be reduced. Attention is also drawn to compliance with the protocol as the key to patient safety. |
Min HJ, Kim HJ, Lee DS, et al., 2019. Republic of Korea | Retrospective cohort study | 535 patients from March 2012 to May 2019 | To determine the incidence and risks of cardiopulmonary arrest (CPA) during IHT accompanied by RRT. | Regardless of the accompaniment, CPA occurs, risk factors include history of myocardial infarction, manual ventilation, 3+ vasopressors. |
Nadig NR, Brinton DL, Simpson KN, et al., 2022. USA | Retrospective quasi- experimental study | ICU patients (n=3774) From 2015 to 2017 | To describe transfer patterns and the impact of transfer duration on patients with acute respiratory failure between intensive care units. | Patients transferred to the appropriate ICU earlier face a 55.8% lower risk of in- hospital mortality. |
Murata M, Nakagawa N, Kawasaki T, et al., 2022. Japan | Systematic review and meta- analysis | 24 studies published up to June 3, 2020. | To examine and describe the safety and side effects during intrahospital transfer of critically ill patients. | Side effects can occur during intrahospital transfer of critically ill patients, and the frequency of critical side effects is relatively low. |
Zirpe KG, Alunpipatthanachai B, Matin N, et al., 2023. India | Electronic research | 365 hospitals in 32 countries from March 1, 2022 to June 30, 2022 | Describing the practice of IHT of neurocritically ill patients in institutions. | Inconsistent standards regarding neurophysiological monitoring during IHT require in-depth monitoring in hospitals and indicate the need for international guidelines for neurocritical care during IHT. |
Table 2. Studies included regarding adult patient intrahospital transfer | ||||
Author, year, country of origin | Type of study | Sample and time of research | Research objective | Conclusion |
Pedrosa L, Hoyos J, Reyes L, et al., 2024. Spain | Cochrane systematic review | Severe brain injury patients (n=27) IHTs (n=67) between January 2017 and January 2019 | To quantify the effect of IHT on brain metabolism by monitoring both hemispheres with bilateral MD. | Brain metabolism is altered after IHT in neurocritically ill patients, without being limited to the affected hemisphere. |
Schmidbauer ML, Wiegand TLT, Keidel L, et al., 2023. Germany | Retrospective cohort study | Patients with subarachnoid hemorrhage (SAH) (n=25) IHTs (n=108) between January 2016 and April 2019 | Analysis of IHTs for demographics, rationale of transport, clinical outcomes, and pre/ post IHT follow-up parameters. | Relevant hemodynamic thresholds were breached in 31.5% of cases, while respiratory complications occurred in 63.9% and neurological complications in 20.4%. |
Beekman R, Crawford A, Mazurek MH, et al., 2022. SAD | Retrospective, single-center study | 22 low-field MRIs were performed in 19 patients resuscitated from cancer from September 2020 to January 2022 | To apply a new approach to assess brain injury after cancer in critically ill patients at high risk for adverse neurological outcome. | Low-field MRI was performed in all patients without interfering with intensive care unit equipment monitoring and there were no safety events. |
Dusse F, Putz J, Bohmer A, et al., 2021. Germany | Prospective observational study | Patient handovers (n=102) 2014 | The aim of this research was to examine the completeness of information transfer and the amount of information. | The completeness of the handover is affected by time pressure, interruptions, and inadequate environment that increase the risk of information loss |
Lin SJ, Tsan CY, Su MY, et al., 2020. Taiwan | Quality improvement study | ICU admission (n=8014) From January 2015 to December 2017 | Implementation of intrahospital transfer protocols in order to improve the safety of mechanically ventilated patients. | The implementation of the established protocol significantly reduced the number and incidence of adverse events. |
Scott J, Dawson P, Heavey E, et al., 2019. United Kingdom | Retrospective study | Incidents (n=278) March 2014 – August 2014, January 2015 – June 2015) | The aim of the research was to analyze the content of incident reports. | Almost 70% of incident reports related to pressure ulcers, falls, medication and documentation errors. |
Table 3. Studies included regarding healthcare professionals’ perspective on intrahospital transfer | ||||
Author, year, country of origin | Type of study | Sample and time of research | Research objective | Conclusion |
Hashemian M, Salami Z, Islam Azizpour, et al., 2023. Iran | Cross- sectional study | Emergency and intensive care nurses (n=288) | To assess the safety of critically endangered patients during intrahospital transfers. | The safety rate is low, and hospitals are obliged to provide a favorable environment for intrahospital transfers by recognizing the risks and taking the necessary measures. |
Temsah MH, Al-Sohime F, Alhaboob A, et al., 2021. Saudi Arabia | Cross- sectional study | Healthcare professionals (n=312) April 2017 | To identify the practices of IHT in different health institutions and to compare the course of transfers in unstable patients compared to stable patients. | Initiatives to improve transfer quality can improve patient safety, and respiratory and hemodynamic complications represent the most significant adverse events. |
Song Y, Zhao Q, Yang M, et al., 2022. China | Cross- sectional study | ICU nurses (n=480) From July to August 2019 | To describe the experiences and attitudes of adult intensive care nurses towards IHT of critically ill patients. | Nurses experienced IHT as a source of stress and increased workload. Checklists and training were useful for patient safety during IHT. |
Bergman L, Chaboyer W, Petterson M, et al., 2020. Sweden | Cross- sectional study | Healthcare professionals in 12 intensive care units in Sweden In the period from February to April 2019, a total of 315 | To develop and evaluate the psychometric properties of a scale for measuring patient safety during the process of intrahospital transfer to ICU. | The results showed acceptable validity and reliability of the scale among a sample of Swedish healthcare professionals. |
Venn AM, Sotomayor CA, Godambe SA, et al., 2021. USA | Single- center study | ER nurses and physicians. 355 (84%) of 400 ED-to-ICU admissions had completed IHT checklists. From July 23, 2019 to July 22, 2020 | To improve the safety of IHT for emergency patients admitted to the pediatric ICU. | The IHT checklist was feasible and associated with improvements in perceived safety and reporting of incident events. |
Lee SH, Wee C, Phan P, et al., 2023. Singapore | Mixed methods study | 6 focus groups with 34 health professionals consisting of doctors and nurses November 2017 | This study reports on the differences in protocols and data elements between receiving and sending transfers in the ICU and the elements that make transfer readiness. | General ward clinicians are more likely to receive ICU patients with complete discharge summaries, while ICU clinicians admitting general ward patients receive significantly less data. |
Mamalelala TT, Schmollgruber S, Botes M, et al. 2023. South Africa | Cross- sectional study | 171 nurses | The aim of this study was to describe nurses’ opinions on the effectiveness of handover between ED and ICU nurses. | The study showed that ER and ICU nurses have significantly different requirements and expectations from handover procedures. |
Based on interviews of healthcare personnel and retro- grade analyzes of IHT, studies have agreed on relative- ly low rates of safety and a structured course of IHT. They show the incidence of adverse events, including significant declines in vital functions. Hospitals strive to be maximally safe institutions; therefore, they must recognize risks and adopt measures to avoid adverse events when providing health care (5, 10). Also, when identifying risk factors, it is important to take into ac- count the patient’s health condition as a predisposing factor. Although adverse events during IHT transfer do not affect the mortality rate, they slow down the course of treatment and prolong the stay in the institution, es- pecially when it comes to patients requiring intensive treatment (11). Their characteristics as such represent risks for adverse events during the transfer, and before considering the other numerous components of the quality and structured course of IHT, according to one study, the incidence of adverse events stagnates with- out significant deviations regardless of the specialized team. In vitally endangered patients, the emphasis in risk identification and prevention is placed on patient evaluation (12). Taking that into account, another study emphasizes that stabilization of the patients before IHT takes place may reduce incidence of adverse events
(13). Also, the training of health professionals plays a
key role if adverse events for the patient occur (14).
IHTs are mostly required for diagnostic purposes and minor procedures. As diagnostic techniques become in- creasingly advanced and include a series of procedures aimed at the best possible clinical assessment, the clini- cian and the multidisciplinary team must always care- fully weigh the benefits of the test compared to the possible complications of the transfer and the procedure itself (15). During IHT, significant hemodynamic thresh- olds can be crossed, leading to an increased risk of vital instability, a series of potential complications and pro- longed hospital stays (16). This is supported by studies that specifically assess neurocritical patients and speak in favor of the need for analysis and improvement of the IHT procedure (17). Studying the metabolism of the brain before and after such migrations, changes are not- ed that are not exclusively related to damaged brain ar- eas (18). In addition, any atypical transfer results in pro- longed treatment (3). The assessment of brain injury is of great importance for the therapeutic approach; there- fore, the implementation of portable diagnostic devices is an important factor in the prevention of complications that may occur during IHT. Research has shown that portable MRI in the assessment of ischemic brain inju-
ry in the ICU did not interfere with the workflow (19). Also, the same research is carried out when it comes to portable CT. Although achieving such conditions repre- sents a financial challenge, research indicates the same effectiveness of the test without interfering with the interventions in the ICU. MSCT, as a frequent and im- portant diagnostic test, in a portable form represents a significant reduction in the need for IHT during inten- sive treatment. Although the number of adverse events did not decrease significantly, the research showed the need for additional analyzes (20). Timely transfers be- tween intensive care units represent an important mo- ment in the course of treatment. A timely transfer be- tween two ICUs reduces the risk of in-hospital mortality by 55.6%, therefore special attention must be paid to ensuring the orderly transfer (21). Also, the analysis of atypical transfers and the network of movement within the hospital are of great importance for identifying risks and ensuring quality (2). In addition to life-threatening events during IHT, pressure ulcers and pressure injuries, falls and errors in treatment and documentation are cit- ed as the dominant incidents. In addition to preventing vital collapses, hospitals strive to maintain the highest possible quality of life, therefore such incidents are en- tirely preventable and should not occur (22).
Clinicians must harmonize and clearly emphasize mu- tual expectations when exchanging information taking different protocols into consideration (23). The integrity of the handover is significantly affected by time pres- sure, interruptions, and inappropriate surroundings (24). Also, using the example of nursing handovers in emer- gency medicine compared with intensive care, we can notice different expectations of the handover content. High quality handover is essential for avoiding adverse effects. According to this study, nurses from different specialties should agree on a structured handover. Al- though this study was conducted in tertiary academic hospital and the results cannot be generalised, it speaks in favor of necessary structure when it comes to final part of IHT: handover (25). Quality improvement initia- tives can affect the reduction of adverse events. Health- care workers’ satisfaction with IHT is related with imple- mentation of formal protocols for IHT and the handover structure. More importantly, better patient outcomes were noted when using formally adapted tools (26). It is recommended to use pre-transport checklists in order to minimize adverse events. Also, minor surgical proce- dures and better bedside diagnostics are highly recom- mended to consider in future (15). Before implementing the protocol, it is necessary to evaluate the one created
![]()
by the health professionals. According to one study, the IHT protocol for Swedish hospitals was created in this way (27). And the very integration of the checklist and protocol proved to be effective in reducing adverse events (28, 29). In order to ensure better management of transfer processes, a network analysis has proven effective. Prior to protocol development, this approach involves a detailed examination of patient movements within the institution. However, the study’s small and specific sample remains a notable limitation (30).
![]()
![]()
An analysis of available literature reveals that ad- verse events during IHTs are a widespread challenge faced by many healthcare institutions. Although such events do not directly affect mortality, they contrib- ute to worse clinical outcomes and longer treatment. They affect hospitals as organizational structures and reduce the quality of healthcare. Research indi- cates the need for extensive analyzes on larger sam- ples. Regardless of the absence of a universally ap- plicable protocol, individual analyzes and guidelines have proved effective. Numerous studies have em- phasized the importance of thoroughly assessing the potential benefits of the transfer against the risks of adverse events. Special attention has been paid to vitally endangered patients as the most sensitive group whose transfers require a multidisciplinary ap- proach and a clearly structured course. Communica- tion and coordination of all team members, as well as the availability of the necessary resources proved to be vital in ensuring the safety of all patients during intrahospital transfers.
Author contributions: Conceptualization (KV, LL); Da- ta Curation (VK, RD); Data Analysis (KV, LL, RD); Writ- ing – Original Draft (KV, LL). All authors contributed to revising and editing the final manuscript
The authors declare that the research was conducted in the absence of any commercial or financial rela- tionships that could be construed as a potential con- flict of interest.
Not applicable.
The authors declare that no financial support was received for the research, authorship and/or publica- tion of this article
![]()
![]()
Veiga VC, Postalli NF, Alvarisa TK, Travassos PP, Vale RT da S, Oliveira CZ de, et al. Adverse events during intrahos- pital transport of critically ill patients in a large hospital. Revista Brasileira de Terapia Intensiva. 2019;31(1):15-
20. https://doi.org/10.1038/s41598-023-41966-w
Zhang C, Eken T, Jørgensen SB, Thoresen M, Søvik S. Effects of patient-level risk factors, departmental al- location and seasonality on intrahospital patient trans- fer patterns: network analysis applied on a Norwegian single-centre data set. BMJ Open. 2022;12(3):e054545. https://doi.org/10.1136/bmjopen-2021-054545
Mendelsohn E, Honeyford K, Brittin A, Mercuri L, Klaber RE, Expert P, et al. The impact of atypical intrahospital transfers on patient outcomes: a mixed methods study. Sci Rep. 2023;13(1):15417. https://doi.org/10.1038/ s41598-023-41966-w
Ott LK, Hoffman LA, Hravnak M. Intrahospital transport to the radiology department: risk for adverse events, nursing surveillance, utilization of a MET and practice im- plications. J Radiol Nurs. 2011;30(2):49-52. https://doi. org/10.1016/j. 2011.02.001
Hashemian M, Salami Z, Islam Azizpour, Alireza Mirzaei. Evaluation of the safety status of intrahospital trans- fer of critically ill patients from the perspective of emergency and ICU nurses: a cross-sectional study in Iran. BMJ Open. 2023;13(10):e072584–4. https://doi. org/10.1016/j.2011.02.001
Kue R, Brown P, Ness C, Scheulen J. Adverse clinical events during intrahospital transport by a specialized team: a preliminary report. Am J Crit Care. 2011;20(2):153-62. https://doi.org/10.4037/ajcc2011478
Yang SH, Jerng JS, Chen LC, et al. Incidence of patient safety events and process-related human failures dur- ing intra-hospital transportation of patients: retrospec- tive exploration from the institutional incident reporting system. BMJ Open. 2017;7(11):e017932. https://doi. org/10.1136/bmjopen-2017-017932
Germack HD, Fekieta R, Campbell Britton M, Feder SL, Rosenberg A, Chaudhry SI. Cooperation and conflict in in- tra-hospital transfers: A qualitative analysis. Nurs Open. 2019;7(2):634-41. https://doi.org/10.1002/nop2.434
Mortensen B, Borkowski N, O’Connor SJ, Patrician PA, Weech-Maldonado R. The relationship between hos- pital interdepartmental transfers and patient expe- rience. J Patient Exp. 2020;7(2):263-9. https://doi. org/10.1177/2374373519836467
Murata M, Nakagawa N, Kawasaki T, Yasuo S, Yoshida T, Ando K, et al. Adverse events during intrahospital trans- port of critically ill patients: A systematic review and meta-analysis. Am J Emerg Med. 2022;52:13-19. https:// doi.org/10.1016/j.ajem.2021.11.021
Ling L, Xia X, Yuan H, Liu S, Guo Z, Zhang C, et al. Ef- fectiveness of the graded transport mode for the intra- hospital transport of critically ill patients: A retrospective study. Front Public Health. 2023;10:979238. https://doi. org/10.3389/fpubh.2022.979238
Min HJ, Kim HJ, Lee DS, Choi YY, Yoon M, Lee D, et al. Intra-hos- pital transport of critically ill patients with rapid response team and risk factors for cardiopulmonary arrest: A retros- pective cohort study. PLoS One. 2019;14(3):e0213146. https://doi.org/10.1371/journal.pone.0213146
Zirpe KG, Tiwari AM, Kulkarni AP, Govil D, Dixit SB, Munjal M, et al. Adverse events during intrahospital transport of critically ill patients: a multicenter, prospective, obser- vational study (I-TOUCH Study). Indian J Crit Care Med. 2023;27(9):635-41. https://doi.org/10.5005/jp-jour- nals-10071-24530
Song Y, Zhao Q, Yang M, Xie X, Gong M, Chen H. Intra- hospital transport of critically ill patients: A cross-sectio- nal survey of Nurses’ attitudes and experiences in adult intensive care units. J Adv Nurs. 2022;78(9):2775-84. https://doi.org/10.1111/jan.15179
Parveez MQ, Yaddanapudi LN, Saini V, Kajal K, Shar- ma A. Critical events during intra-hospital transport of critically ill patients to and from intensive care unit. Turk J Emerg Med. 2020;20(3):135-41. https://doi. org/10.4103/2452-2473.290067
Schmidbauer ML, Wiegand TLT, Keidel L, Zibold J, Dimitriadis
K. Intrahospital transport of critically ill patients with su- barachnoid hemorrhage-frequency, timing, complications, and clinical consequences. J Clin Med. 2023;12(24):7666. https://doi.org/10.3390/jcm12247666
Zirpe KG, Alunpipatthanachai B, Matin N, Gulek BD, Blissitt PA, Palmieri K, et al. Benchmarking hospital practices and policies on intrahospital neurocritical care transport: the safe-neuro-transport study. J Clin Med. 2023;12(9):3183. https://doi.org/10.3390/jcm12093183
Pedrosa L, Hoyos J, Reyes L, Mosteiro A, Zattera L, Topce- zewski T, et al. Brain metabolism response to intrahospi- tal transfers in neurocritical ill patients and the impact of microdialysis probe location. Sci Rep. 2024;14(1):7388. https://doi.org/10.1038/s41598-024-57217-5
Beekman R, Crawford A, Mazurek MH, Prabhat AM, Chav- va IR, Parasuram N, et al. Bedside monitoring of hypoxic ischemic brain injury using low-field, portable brain ma- gnetic resonance imaging after cardiac arrest. Resuscita- tion. 2022;176:150-8. https://doi.org/10.1016/j.resusci- tation.2022.05.002
Yoann L, Clément M, François E, Elise B, Hubert S, Jean- Cristophe F, et al. Implementation of portable head CT
imaging in patients with severe acute brain injury in a French ICU: a prospective before-after design pilot stu- dy. Sci Rep. 2022;12(1):20846. https://doi.org/10.1038/ s41598-022-25263-6
Nadig NR, Brinton DL, Simpson KN, Goodwin AJ, Simpson AN, Ford DW. The impact of timing on clinical and econo- mic outcomes during inter-icu transfer of acute respira- tory failure patients: Time and tide wait for no one. Crit Care Explor. 2022;4(3):e0642. https://doi.org/10.1097/ CCE.0000000000000642
Scott J, Dawson P, Heavey E, Brún AD, Buttery A, Wa- ring J, et al. Content analysis of patient safety incident reports for older adult patient transfers, handovers, and discharges: do they serve organizations, staff, or pati- ents? J Patient Saf. 2021;17(8):e1744-58. https://doi. org/10.1097/PTS.0000000000000654
Lee SH, Wee C, Phan P, Kowitlawakul Y, Tan CK, Mukho- padhyay A. Readiness for transfer: a mixed-methods study on ICU transfers of care. BMJ Open. 2023;13(5):e064492. https://doi.org/10.1136/bmjopen-2022-064492
Dusse F, Pütz J, Böhmer A, Schieren M, Joppich R, Wappler
F. Completeness of the operating room to intensive ca- re unit handover: a matter of time? BMC Anesthesiol. 2021;21(1):38. https://doi.org/10.1186/s12871-021-
01247-3
Mamalelala TT, Schmollgruber S, Botes M, Holzemer W. Effectiveness of handover practices between emer- gency department and intensive care unit nurses. Afr J Emerg Med. 2023;13(2):72-7. https://doi.org/10.1016/j. afjem.2023.03.001
Temsah MH, Al-Sohime F, Alhaboob A, Al-Eyadhy A, Alja- maan F, Hasan G, et al. Adverse events experienced with intrahospital transfer of critically ill patients: A national survey. Medicine (Baltimore). 2021;100(18):e25810. https://doi.org/10.1097/MD.0000000000025810
Bergman L, Chaboyer W, Pettersson M, Ringdal M. Deve- lopment and initial psychometric testing of the Intrahos- pital Transport Safety Scale in intensive care. BMJ Open. 2020;10(10):e038424. https://doi.org/10.1136/bmjo- pen-2020-038424
Venn AM, Sotomayor CA, Godambe SA, Vazifedan T, Jennings AD, et al. Implementation of an intrahospital transport checklist for emergency department admissi- ons to intensive care. Pediatr Qual Saf. 2021;6(4):e426. https://doi.org/10.1097/pq9.0000000000000426
Lin SJ, Tsan CY, Su MY, Wu CL, Chen LC, Hsieh HJ, et al. Improving patient safety during intrahospital tran- sportation of mechanically ventilated patients with critical illness. BMJ Open Qual. 2020;9(2):e000698. https://doi.org/10.1136/bmjoq-2019-000698
Secor EA, Hamilton D, D’Huyvetter C, Salottolo K, Bar- Or D. Network analysis examining intrahospital traffic of patients with traumatic hip fracture. J Healthc Qual. 2023;45(2):83-90. https://doi.org/10.1097/ JHQ.0000000000000367
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;372:n71. https://doi.org/10.1136/bmj.n71