
![]()
![]()
1 Sara Marinac
2 Vesna Turuk
1 Department of Neonatology and Neonatal Intensive Care Medicine, University Hospital Centre Zagreb, Zagreb, Croatia
2 University of Applied Health Sciences, Zagreb, Croatia
![]()
![]()
Vesna Turuk
University of Applied Health Sciences Mlinarska 38, Zagreb, Croatia
![]()
https://doi.org/10.24141/2/7/1/3
![]()
![]()
![]()
![]()
Conjoined ("Siamese”) twins are one of the rarest con- genital anomalies with an incidence of about 1.47 per 100,000 births in the Western world. This rare natu- ral phenomenon is present in only 1% of monozygotic twins, i.e., 0.05% of live births. Most of them are still- born (40-60%) or die early in life. The majority of live births are female (75%), which is why the female kar- yotype is considered to be beneficial in terms of sur- vival. Conjoined twins are created when the zygote begins to separate after 13 days post-fertilization, at a time when the so-called embryonic disc has already been formed. Instead of producing two separate em- bryos, this late separation causes incomplete separa- tion of the embryos. The name comes from conjoined twin brothers Chang and Eng Bunker, who were born in Siam. Surgical separation of conjoined twins is usu- ally a very demanding and complex procedure, and often not even possible. Survival after separation de- pends on the type of connection.
This paper presents the case of conjoined twins who were born at 33 weeks. At 11 weeks of pregnancy, the doctors suspected that the twins were joined ventrally (omphalopagus – twins joined at the abdo- men). The diagnosis was confirmed by fetal MRI at 21 weeks. Separation was indicated at the age of 45 days and a combined body weight of 4,700 g. Long postoperative recovery and treatment lasted three months and was complicated by infections and prob- lems with the healing of the surgical wound of one of the twins. Treatment and recovery required a mul- tidisciplinary approach and a well-educated team of doctors and nurses.
![]()
![]()
Conjoined twins are twins who are physically fused in the womb and consequently at birth. The first mention of conjoined twins dates back to the Neo- lithic period (1). The most common etiology of con- joined twins is partial fission or secondary fusion. Both of these processes can be used to explain the embryological and anatomical findings observed in conjoined twins (2). Conjoined twins are the result of axis splitting or duplication that occurs after 13 days post-fertilization. They are described according to the site of fusion and are a rare atypical presen- tation of symmetric monozygotic twin pregnancies. They are of the same sex and karyotype. They are more common in women with a ratio of men to wom- en of 1:3. They are the result of incomplete embryo splitting into two separate twins after 12 days post- fertilisation. Conjoined twins are more often female. They are classified according to the point of fusion: ventral-rostral, caudal, lateral and dorsal. Among conjoined twins, Thoracophagus is the most com- mon type (3,4). Traditional healthcare strategies may require modification to meet the unique care needs of conjoined twins. Areas of focus include ensuring privacy, designing appropriate housing units to meet space and equipment needs, staffing considerations, and adaptations to typical neonatal intensive care interventions. Caring for conjoined twins is a com- plex process and the role of the nurse has an impor- tant impact on the overall outcome. Even basic and
routine nursing tasks must be adapted to meet the needs of these unique patients (5).
Conjoined twins are a rare embryological develop- mental disorder of unclear etiology. The condition itself implies malformations and is associated with secondary changes associated with abnormally con- nected organs and the superimposed effects of ab- normal hemodynamics. The proposed defect mech- anisms cannot explain the changes in the normal developmental process, whereby a pair of monozy- gotic twins do not separate from each other and con- tinue their normal embryological development (6). The rarity and complexity of this condition present a challenge for prenatal planning and postnatal care. Medical, imaging, and surgical advances have led to earlier, more accurate depictions of anatomy, and as a result, have allowed more time for the team of pro- fessionals to prepare for their complex care (7).
Since ancient times, conjoined twins have captured the attention and fascination of people around the world. Over the centuries they have been worshipped as gods, feared as monsters, and paraded before curi- ous crowds for entertainment. They were integrated into the myths and legends of many ancient civili- zations, especially Janus, the ancient Roman god of beginnings and ends. For centuries, people consid- ered conjoined twins, as well as children with birth defects, to be a bad omen or a sign of God’s wrath (8). Probably one of the first documented cases was

Figure 1. “Siamese twins” - brothers Chang and Eng
Source: https://www.abc.net.au/news/2016-11-14/chang-and-eng-bunker-the-original-siamese-twins/7992942
a pair of conjoined twins born in Isle-Brewers, Eng- land, joined at the back from the middle of the chest to near the lumbar region part. Anecdotal reports of live conjoined twins in European medical history date back more than 1,000 years, but the first well-known case was not documented until 1811 when 2 boys
- Chang and Eng - were born in Bangkok, Thailand, attached at the sternum and they were called “Sia- mese twins” (Figure 1). As they travelled the world with Barnum’s Circus, they consulted with a multi- tude of doctors. Everyone, including Rudolf Virchow, concluded that separation would be fatal for both of them (9).
The exact incidence of conjoined twins has not been determined, and the estimated frequency varies in the literature. All conjoined twins are monoamniotic, monochorionic and monozygotic twins. Conjoined twins occur in 1.6% of all human pregnancies, of which 1.2% are fraternal and 0.4% are monozygotic. Monochorionic-monoamniotic twins account for less than 1% of identical twins, and conjoined twins are even rarer, occurring in approximately 1 in 50,000– 100,000 and 1:600 live births. Conjoined twins are three times more common in female fetuses than in male fetuses. It is believed that 1 in 40 monozygotic twins fail to separate, producing conjoined twins. There was a reported incidence of 1:14,000 live births in India and Africa and 1:250,000 live births in Europe and the USA, suggesting an increased inci- dence in the black population (10). More recent stud- ies on the epidemiology of conjoined twins are rela- tively rare, but the prevalence does not appear to be significantly different (1.02–1.34 per 100,000 births) in Western populations. However, an increased prev- alence of 3.27:100,000 births and 2.85:100,000 births was reported in two studies on the Chinese population from the same Surveillance Program at different times (6).
The anatomical structure and physiological function- ing of the female reproductive system are predis- posed for the conception of one embryo which, after implantation, develops into a fetus and is born natu- rally as a normal newborn at full term. Sometimes, however, various disorders can disrupt this sequence of processes. A special example of such a disorder
is multiple pregnancies, which are often and incor- rectly called twin pregnancies because there can be more than two fetuses. Ovulation disorders can lead to the release of several eggs that, when joined with sperm, form independent zygotes and then pol- yzygotic fetuses. Embryonic regulation is a specific characteristic of early embryo development. It can lead to the development of genetically identical (mo- nozygotic) twins. This phenomenon is not treated as a pathology, especially since further embryonic de- velopment, birth and postnatal development are of- ten normal (11). It is now generally accepted that a human embryo can divide and form into monozygotic or identical twins at one of three stages of develop- ment. After fission or cleavage, two genetically iden- tical embryos would be expected and after zona ly- sin, each would implant and develop as two distinct, although genetically identical, embryos (12).
Currently, the generally accepted and prevailing the- ory that could explain the origin and development of fused fetuses is the fission theory. It is assumed that during gastrulation when the embryo still has the shape of an elliptical disc, the disc spontaneously cleaves incompletely along the cephalocaudal axis. The process of embryonic regulation creates con- joined twins. They are characterized by homologous connection, which means that both individuals share the same organs, e.g., head-to-head or back-to-back. Fragmentation of the embryonic disc and separation of tissue elements can be caused by environmental factors, cell adhesion disorders or increased geneti- cally conditioned apoptosis, i.e., cell death. An alter- native theory that explains the origin of conjoined twins is the spherical theory. It is assumed that the embryonic discs, which are formed after the com- plete cleavage of the embryo in the early stage of development, may have a common yolk sac. The cells that form it can “swim” or “float” on its surface and rejoin, usually endodermally, thus creating ventrally conjoined twins. On the other hand, dorsally con- joined twins are the result of ectodermal fusion due to the approximation of embryonic discs that share a common amniotic cavity at an early stage (11).
The most common case of conjoined twins is two conjoined children of a similar stage of development. In general, conjoined twins are divided into ven- trally fused conjoined twins (approximately 69.3% of cases) and dorsally fused conjoined twins (5.4%).
Figure 2. Ventrally fused conjoined twins
Source: https://www.researchgate.net/figure/Types-of-twins-according-to-Spencer-O-omphalopagus-T-thoracopagus-Ce-cephalopagus-I_fig2_8432231
The remaining types include connections of a non- specific nature (21.4%) and the so-called parasitic twins (3.9%), i.e., those characterized by significant morphological disproportions. The nomenclature as- sociated with the pathologies observed in the case of joined fetuses is based on the morphology of the connection. Ventrally conjoined twins can be divided into cephalically conjoined, which include thoracopa- gus (42%), cephalopagus (5.5%) and omphalopagus (5.5%). An example of caudal fusion is ischiopagus (1.8%), and lateral fusion parapagus (14.5%) (Figure 2) (13).
Ventrally fused conjoined twins initially share a com- mon yolk sac that participates in the development of the intestines, liver and pancreas. They usually share a common peritoneal cavity and umbilical cord. Their hearts can be shared or separated depending on the level of fusion. The thoracopagus type is formed by fusion at the cardiac primordium. The connection in- cludes the chest and the upper part of the abdominal cavity. In this case, numerous common organs pre- vent separation. The cephalophagous type develops by initial fusion on the oropharyngeal membrane at the anterior part of the embryonic disc. After that, it stretches from the top of the head to the navel. In this case, the trunks of both fetuses share the head and chest. The prognosis for their survival and devel- opment is very unfavourable (12). The omphalopa- gus type develops by the fusion of the primordial di- aphragm. The connection includes the chest and the upper part of the abdominal cavity. The ischiopagus type is associated with a common cloacal membrane and the development of the hindgut and rectum. It
also includes the musculoskeletal system of the back of the body. Such fusion can also be found in the lower part of the abdominal cavity and the area of the urogenital tract. Fusion usually does not involve critical organs and newborns can be effectively sepa- rated. The parapagus type develops by fusion of the anal primordium, often retaining two notochords, and eventually the lower spinal segments. The connec- tion involves the pelvis and torso to varying degrees; there are one or two heads and two faces (13). Dor- sally conjoined twins are divided into the following types: craniopagus (3.4%), rahipagus (1.0%) and py- gopagus (1%). These twins share a part of the axial nervous system that originates from the neural tube (Figure 3) (7).
Figure 3. Dorsally fused conjoined twins
Source: https://www.researchgate.net/figure/Types-of-twins-according-to- Spencer-O-omphalopagus-T-thoracopagus-Ce-cephalopagus-I_fig2_8432231
The spine and its muscles are common, but there are two abdominal cavities. Umbilical cords are usually separate. The craniopagus type develops with an
initial fusion in the region of the anterior neural fora- men that ultimately includes the cranial vault. The rachipagus type develops from the fusion of the cen- tral part of the neural tube that includes the spine and its muscles. The pygopagus anomaly is formed by the fusion of the caudal segments of the neural tube in the area of the posterior neural opening and ultimately involves the sacrum and coccyx with the pelvic muscles. It is important to emphasize that all types of conjoined twins have a common etiology (7).
Developments in imaging and radiology have ena- bled physicians to diagnose and assess the extent of fusion at an early developmental stage in most cases of conjoined twins. It is now possible for the medical team to more accurately predict the outcome and adequately counsel families to help them decide whether to continue with the pregnancy or opt for early termination. Prenatal assessment is currently primarily performed using ultrasound, with the ad- dition of colour Doppler imaging and a three-dimen- sional ultrasound, which help in establishing an ac- curate diagnosis (8). Currently, prenatal ultrasound is commonly used to diagnose conjoined twin preg- nancies and can be performed as early as 12 weeks of pregnancy. However, a detailed scan at 20 weeks gestation gives a reasonable estimate of the extent of the fusion and any other problems. The non-inva- sive nature and safety of this procedure make it the modality of choice for early in-utero diagnosis. This technique uses the amniotic fluid’s ability to act as a buffer during scanning. When appropriate, trans- vaginal ultrasound is also recommended. According to recent studies, prenatal fetal MRI can add informa- tion to help define the exact anomalies and connect anatomies between fetuses, as a result of its higher resolution, lack of ionizing radiation and its non-inva- sive nature. They are widely used to delineate ana- tomical details, especially the cardiovascular system. A detailed examination of the heart is particularly important because the prevalence rate of congenital heart abnormalities in conjoined twins is high (14). Correct diagnosis is also an important aspect in plan- ning the obstetric care of conjoined twins, as are the decisions about the method and timing of delivery. Early diagnosis of conjoined twins will then allow for better management including preventing premature birth and allowing the fetuses to continue their nor- mal development. The method of choice for deliver-
ing conjoined twins is a Cesarean section. Needless to say, the more one knows about the twins before the operation, the better the outcome of the separa- tion procedure will be (15).
If the diagnosis is made in the first trimester, the twins should be delivered by a Cesarean section at or near the hospital where the separation will take place. However, in many cases, the condition is not discovered until labour is obstructed (16). Conjoined twins fall into one of three groups - namely newborns who do not survive birth (and those who die shortly after birth), infants who survive till elective surgery and infants who require emergency surgery. Elective separation is possible in omphalopagus, pygopagus and some craniopagus, and thoracopagus twins. Separation is not possible with cephalopagus, para- pagus and rahipagus twins. Urgent separation may be necessary when there is damage to the connect- ing bridge (omphalopagus), where one twin threat- ens the life of the other (complex congenital heart disease, cardiomyopathy, sepsis), when the condi- tion of both twins deteriorates due to hemodynamic and respiratory disorders (typically thoracopagus) or where the condition of one of the twins is incompat- ible with life (anencephalic, stillborn), and the other has good prospects for survival (17).
As a result of the multiple organ abnormalities of conjoined twins, it is necessary to perform a thor- ough examination of each organ system. The most critical organ that determines the prognosis of sur- gical separation is the heart. Parts of the gastroin- testinal (GI) system are usually shared in most cases of conjoined twins, except in craniopagus twins. An adequate examination of the digestive tract can be done by applying dyes at a separate time intervals to understand which structures are being divided. Ultrasound, 3D-MRA and radioisotopes can be used for analysis in the presence of a common pancreas and biliary system, which are often found in thora- copagus and omphalopagus twins. Cystoscopy has become a popular approach to examining the geni- tourinary system in cases involving the common bladder, rectum, and/or vagina. It is also important to assess the kidneys, including their number, location, and degree of fusion. Ultrasound and MRI are com- monly used for such purposes. In male twins, joint use of the genitals, scrotum and testicles should be evaluated (18).
During the separation procedure, great attention is paid to anesthesia, breathing and hemostasis. Certain experts are assigned to each twin separately, along with a joint team coordinator. Due to shared circula- tion, poorer cardiac function, and unpredictability of reactions to drugs, administration of anesthesia dur- ing the separation procedure can be difficult. Endotra- cheal intubation is strongly recommended to main- tain adequate respiratory gas exchange. However, it can be difficult to intubate thoracopagus twins (10). Cross-circulation between conjoined twins has signif- icant implications for anesthetic pharmacology and resuscitation. Where cross-circulation is imbalanced, significant end-organ (cardiac, renal, and respiratory) failure can occur. It should also be recognized that the degree of cross-circulation is dynamic and de- pends on the relative systemic vascular resistance of both twins. Although dosing of anesthetics, antibiot- ics, and analgesics is often based on weight (using half the combined weight as a standard), effects can be erratic. Induction of anesthesia should be simul- taneous since inhalation of volatile substances can cause complete, no or some effect on the other twin.
Heparin dosing before cardiopulmonary bypass may be compromised by unequal flow distribution be- tween the twins. Careful angiographic imaging of the cross-circulation is necessary to assess the fraction of cardiac output shared between twins because the survival of one twin may depend on the circulation of the other (16). Due to the possibility of large blood loss, it is very important to maintain adequate tissue perfusion. Conjoined twins usually have critical en- ergy needs due to significant cardiopulmonary and metabolic abnormalities. Therefore, dextrose and isotonic electrolyte solutions can be administered intravenously. When necessary, palliative procedures including amputations, draining colostomies and il- eal conduits are performed. Complications such as arrhythmia, cardiac arrest and vascular thrombosis may occur during surgical procedures. There is also an increased risk of anesthesia complications, hypo- thermia, and ventilatory failure due to the need for prolonged anesthesia. Greater radiation exposure and a greater need for contrast administration also require careful consideration (19).
After the surgical separation, the twins need inten- sive treatment and care. They should be transported to intensive care units and constantly monitored for signs of bleeding, hypotension, hypothermia, hy- pocalcemia, electrolyte loss, hypoxia, and acid-base
imbalance. Cardiovascular, pulmonary and renal func- tional indicators should be continuously recorded to prevent any complications. Mechanical ventilation may be necessary for twins with severe respiratory distress. A review of the literature indicates that car- diovascular and respiratory failure are still the two major risk factors for twin death after separation. The stress of long-term treatment and surgery puts the twins at risk for infections and delayed wound healing. Therefore, central venous lines should be maintained for rapid access to provide intravenous boluses of fluids, blood, parenteral nutrition, or an- esthetics. Additional surgical procedures may be re- quired to repair any other visceral abnormalities (8).
Health workers often face ethical dilemmas in their practice. However, conjoined twins bring their own unique set of ethical challenges. Already at the initial diagnosis, the decision to continue or terminate the pregnancy is often difficult. However, the real chal- lenge begins at birth, when the decision is made for or against separation. The main goal of the separa- tion procedure is not only to save lives but also to improve the quality of life of the twins. Except emer- gencies that require separation, this notion assumes that twins do not have a fulfilling life if they are not separated (10). Cases where there is significant or- gan sharing, yet two different functioning brains, are philosophically and ethically challenging. This is because they raise questions about a person’s iden- tity, whether they are identical to something psycho- logically or biologically, they force a person to decide whether what matters from an ethical point of view is the biological life of organisms or the existence of consciousness or mind. They raise questions about when, if at all, it is morally acceptable to sacrifice one person to save another. They force you to think about the conditions of organ ownership and the justifica- tion of organ removal for transplantation that causes the death of the donor. They raise questions about who should make decisions about life-threatening treatments when patients themselves cannot decide (20). These cases raise serious moral issues about whether surgical separation should be attempted when extensive organ overlap makes the conjoined twins’ life prospects poor, but their surgical separa- tion is medically difficult and risks worsening the life prospects of at least one of the twins (14). If the necessary operation is easily performed and without
risk, there is a strong moral reason to perform it, since it is likely to improve the life prospects of the twins even more, since conjoining in all its forms brings some disadvantages, such as reduced privacy and exposure to public opinion. curiosity. Such cases can conditionally be called win-win cases because the life prospects of both twins are improved by separa- tion (21). This case report was conducted with the permission of the parents and in accordance with the guidelines for the safety of persons participating in such research, including the Declaration of Helsinki.
The specificities of nursing care of conjoined twins will be shown in the example of the girls born in the 33 weeks of gestation who were admitted to the Department of Neonatology and Neonatal Intensive Care of the Zagreb Clinical Hospital Center 65 min- utes after birth. Treatment and care for conjoined twins involve patient-centred care, a multidiscipli- nary team consisting of neonatologists, intensivists, surgeons, cardiologists, radiologists, pulmonologists, gastroenterologists, and a nurse is an indispensable member of this team. Likewise, caring for conjoined twins requires continuity of care, consistent commu- nication, and the development of trust and comfort between staff and family.
The girls V. and K. T. were born from the third, spon- taneously conceived and regularly controlled preg- nancy in which a twin pregnancy was monitored from the 11 weeks gestation when it was suspected that they were twins joined in the abdominal area. At 21 weeks gestation, a fetal MRI was performed, when two fetuses were confirmed to be joined ventrally by a common liver (fused in the abdominal area with the largest craniocaudal diameter of 4 cm – omphalopa- gus type). The thorax and pelvis of the fetus were distinctly separated. Every fetus had properly devel- oped upper and lower limbs. Separate stomachs were observed, but this method cannot confirm or exclude the existence of a common biliary system (gallblad- ders were not observed with certainty) or other parts of the alimentary canal. Dilation of the intrahepatic bile ducts was not observed. The diaphragm was not visible as an anatomical structure, but its develop- ment was certain given the clear separation of the
anatomical structures of the abdomen from those of the thorax, without signs of diaphragmatic hernias. Nevertheless, a common diaphragm in the ventral part of both fetuses could not be ruled out. A sepa- rate urinary bladder was visible in both fetuses, as well as separate hearts with a regular display of col- lapsed lung parenchyma. As far as was available for analysis, there was one placenta, and one umbilical cord that was traced to the caudal part of the ventral junction. With this presentation, it was not possible to analyze the details of the blood flow of the fe- tuses, that is, to confirm or exclude the involvement of large blood vessels, especially veins, in the area of the omphalopagus. The presentation of cord paren- chyma of both fetuses was regular.
Fetal echocardiography in the 29 and 33 weeks ges- tation showed regular morphology of the hearts of both fetuses. On 10 January 2019 (GD 32+3 weeks), the mother was hospitalized at the Department of Pregnancy Pathology of the Sveti Duh Clinical Hos- pital due to planned preparations for the termination of pregnancy, and on 16 January 2019 at 9:41 a.m., 2 female premature babies were born by Cesarean sec- tion, fused in the area of the lower part of the thorax and abdomen, with a combined birth weight of 3800 grams. The first twin was 43 cm long, with a head circumference of 29 cm, Apgar 7/8, cyanotic, not breathing on her own, with a heart rate <100/min, intubated, ventilated manually with a self-expanding balloon, and a peripheral venous line was installed. The second twin was 41 cm long, with a head circum- ference of 30 cm, Apgar 6/7/8, cyanotic, not breath- ing independently, with a heart rate <100/min, intu- bated and ventilated manually with a self-expanding balloon, and a peripheral venous line was placed and adrenaline administered due to bradycardia. For fur- ther treatment and care, the conjoined twins were transported in a transport incubator to the Clinical Hospital Center Zagreb, Department of Neonatology and Neonatal Intensive Care Medicine.
Upon arrival at the department, the first twin, V.T., was orally intubated, manually ventilated, eupnoeic, did not use auxiliary respiratory musculature, had lit- tle spontaneous motor activity, blood oxygen satu- ration (SpO2) was 90%, heart rate 140/min, blood pressure 45/24 (33) mmHg, and body temperature measured cutaneously was 35.1°C. The second twin, K.T., was orally intubated, manually ventilated, cy-

Figure 4. Conjoined twins after admission to the Department
Source: author
anotic, tachydyspnoic, retracting the intercostal spaces, spontaneous motility was absent, SpO2 79%, heart rate was 124/min, blood pressure 67/54 (61) mmHg, and body temperature measured cutaneously was 35.2°C. The twins were joined to each other ven- trally, in the anterior medial line from the xiphoid to the outlet of the umbilical cord. On palpation, it ap- peared that the twins were fused in the area of the xiphoid/lower part of the sternum. The twins were cared for by a single nurse whose assessment provid- ed valuable insight to the medical team in identify- ing clinical patterns, recognizing subtle changes and gaining a more meaningful understanding of the ob- served behaviour. When caring for conjoined twins, it is important that nurses caring for them understand their anatomy and expected physiology immediately after birth and are prepared for emergencies. Having a child hospitalized with complex medical problems causes significant stress on the family. The consist- ency of nurses in their approach and interventions provides an opportunity to observe family dynamics. This helps the care team optimize communication, manage parent education and understand coping mechanisms. The nurse is often a strong, supportive advocate for patients and families and can identify and seek out helpful resources (7).
The twin girls were placed in an incubator and con- nected to mechanical ventilation. The most common- ly used vascular approaches in neonatal care are the peripherally inserted central catheter (PICC) and the umbilical catheter (22). Due to the obvious impossi- bility of placing an umbilical catheter, girls V. and K. were inserted with PICC catheters.
Trophic feeding was started on the fourth day using breastmilk, with a gradual increase in the volume of the meals, which both twins tolerated adequately. On the twelfth day after being born, due to the ne- crotizing enterocolitis in the first twin, the enteral intake of both twins was stopped and antimicrobial therapy was started, which was quickly followed by a good clinical response and normalization of inflam- mation parameters. Due to the intertwin transfusion syndrome (cross-mixing of circulation between twins via a portosystemic shunt in the common liver paren- chyma, proven by MSCT angiography), progressive arterial hypertension and polyuria (diuresis 308 mI/ day) were observed in the one twin, and oliguria (diu- resis 42 mI/day) in the other twin.
Serum electrolytes, creatinine and urea, due to abun- dant mixing of blood, were repeatedly uniform and within reference values in both twins. However, creatinine clearance in twin K. on the 30th day of life was 54 ml/min/1.73 m2, and in twin V. 32 ml/ min/1.73 m2. The twins were connected to a moni- tor and the heart rate, blood pressure, number of res- pirations and blood oxygen saturation of each twin were recorded in the nursing documentation, and the laboratory findings from the venous blood sample were regularly checked. Ultrasound of the abdomen and colour doppler of the splenoportal basin were performed, showing 4 kidneys without signs of hy- dronephrosis, 2 separate urinary bladders, 2 spleens, 1 liver with normal echogenicity without dilatation of the bile ducts, 2 portal veins and normal hepatic arteries and veins. The gallbladder was shown only in the second twin. As already mentioned, the girls were on mechanical ventilation, each on their ven- tilation parameters, and the nurse monitored the respiratory status every day and periodically, if nec- essary, performed aspiration of the endotracheal tube. Endotracheal tube aspiration is a routine and common procedure in the intensive care unit to re- move secretions and maintain airway patency so that oxygenation and ventilation in an intubated child can

Figure 5. View of conjoined twins after mechanical ventilation
Source: Author
be optimized. However, tube aspiration can cause hypoxia due to aspiration of oxygen from the lungs and alveolar collapse (24). Therefore, it is important to carry out the aspiration procedure in an adequate way. It is important to choose the appropriate size of the aspiration catheter, which should be one-third the size of the diameter of the inner lumen of the tube. Aspiration is performed by two nurses; one who performs aseptic aspiration and one that as- sists. The aspiration nurse advances the aspiration catheter to a predetermined length, ensuring that the catheter is only passed through the length of the tube. Applying negative pressure, the nurse gently rotates the catheter as they pull it out of the tube. The duration of negative pressure should not exceed 6 seconds to prevent hypoxemia. In order to prevent accidental extubation, the assisting nurse gently holds the child’s head in a still position and perfuses the child between two aspiration procedures with a manual balloon.
When the procedure is complete, the nurse recon- nects the ventilator tubing. After that, the nurse as- pirates the child’s nose and oral cavity to free them of secretions using a 6- or 8-gauge probe catheter for this procedure. It is important to observe the child’s physiological parameters after aspiration. If closed suction is used for aspiration, the procedure is per- formed by one nurse because the aspiration catheter is protected in a foil that ensures sterility and there is no need to separate the child from the respirator. The method and duration of the procedure are the same as for open aspiration (25).
On the fifth day after birth, following the application of surfactant, the girls were taken off the ventilator, and respiratory support was continued with non-in- vasive mechanical ventilation (Figure 5).
Non-invasive mechanical ventilation has been in use for pediatric patients for many years. Historically, continuous positive airway pressure and bilevel posi- tive airway pressure modes have been used for res- piratory diseases, including neonatal apnea, bronchi- olitis, asthma, and pneumonia. The newest type of non-invasive respiratory support is the application of a high flow of air and oxygen to a nasal cannula (high flow nasal cannula - HFNC), which has gained popu- larity in the last few years and its use is justified in the literature. Studies have shown that this method of respiratory support can reduce the need for intu- bation and ventilation, reduce the length of intensive care days and increase the comfort of the newborn. The skin, especially of young infants on long-term therapy, may be compromised under the interface due to pressure on the skin. Prevention of skin dam- age can be achieved by using a skin protectant (26). Maintaining the skin integrity of conjoined twins can be challenging due to limited positioning and mobil- ity. During the care of the twins V. and K., a foam mattress was used to protect the skin from pressure injuries, and the twins were successfully placed on their mother’s lap for bonding and social interaction. An important component of achieving the mothering role is bonding with infants through direct physical interaction, encouraging talk, touch, physical nurtur- ing and holding as early and as often as possible.
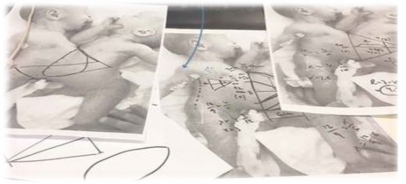
Figure 6. The plan for separating the twins
Source: Author
With conjoined twins, enabling such interaction may be more feasible when they are younger and small- er in size, making the early days and weeks crucial for optimizing the mother’s confidence. Foam packs helped reduce the redness of bony prominences. Gel pads have also been useful during hospitalization in reducing pressure on bone prominences. Reposition- ing and turning are imperative to prevent pressure injuries and maintain comfort. The twins’ positions were changed every three hours. A key consideration in repositioning is maintaining twin identification. The twins needed to remain on their designated side of the bed to ensure proper identification. During hospitalization, the first twin V. T. urinated sparingly, had no bowel movement and developed necrotizing enterocolitis (NEC), which was treated conservative-
ly. The second twin K.T. urinated profusely (dialyzes the first twin), and a native CT showed a larger heart compared to the first twin, which was a consequence of hemodynamics, and she developed hypertension. On February 20, 2019, the medical advisory board held a meeting with the parents with the aim of mak- ing a decision on separation, but the decision was not reached (Figure 6). Six days later, at the re-meeting of the council, an agreement was reached on the sur- gical procedure due to the threatening decompensa- tion of the second twin’s heart, and the separation procedure was agreed upon for March 2, 2019.
The conjoined twins were transported to the operat- ing room on March 2, 2019, at 7 in the morning (Fig- ure 7).

Figure 7. Separation surgery
Source: Author

Figure 9. The first twin after arriving at the Department after surgery
Source: Author
The first twin kept a common part of the intestine from the duodenum to the omphalomesenteric duct, and because of NEC, a subtotal colectomy was per- formed and an ileostomy was formed. The intestinal continuity was established after 2, and the final clo- sure of the abdominal wall after 4 months. The sec- ond twin kept a part of the remaining intestine (the duodenum before the joint part was connected to the ileum, and the abdominal wall was closed using Vacuum-Assisted Closure (VAC). The separated twins were transported back to the Department around 10 p.m.
After being admitted from the operating room, the girls were each placed in their incubator and cared for by two nurses. Continuous monitoring and meth- ods of intensive treatment were carried out, which included the use of antimicrobial and antimycotic therapy, parenteral nutrition and nursing care. After separation, the other twin established adequate diu- resis and gradual regression of arterial hypertension and hypertrophic cardiomyopathy occurred. During the course of stay after the operation, there was re- peated appearance of fresh blood in the stool and abdominal distension, which normalized only after
the use of therapy and a semi-elemental milk formula (Alfare).
During the care of the first twin, the nurse paid spe- cial attention to the surgical wound and ileostomy due to the development of possible complications (Figure 9). The appearance of the ileostomy was as- sessed by observing the colour of the stoma and the surrounding skin. A red or dark pink stoma indicates adequate blood supply, while pale pink indicates reduced hemoglobin or poor perfusion, and grey to black indicates ischemia and potential necrosis, and urgent surgical examination is required. It is also necessary to assess the protrusion of the ileostomy, which is normally 0.5 - 1 cm above the skin. A retract- ed stoma indicates complications and is located be- low the level of the skin, as well as a prolapse, which indicates a protrusion of the stoma more than 2-3 cm above the skin (27). An infant with a formed ileos- tomy requires frequent and regular assessment of fluid and electrolyte status to prevent complications. Sodium is crucial for growth and infants with per- sistent sodium deficit are at risk of reduced growth and cognitive dysfunction. It is necessary to check serum electrolytes, urea and creatinine at least once a day until it stabilizes, then once a week until rean- astomosis. More frequent monitoring depends on the child’s weight gain, stoma losses, age, electrolyte stability and general condition. Sodium in the urine should be checked once a week. In infants with good renal tubular reabsorption, urinary sodium is the best measure of total body sodium and level of depletion. However, results can be misleading in premature in- fants and those with kidney disease. A low level of sodium in the urine (<20 mmol/L) is an indication to start taking nutritional supplements. However, most neonates with a stoma will need a supplement of 2-4 mmol/kg/day, which implies the addition of 3% sodi- um intravenously and modification of total parenteral nutrition (28). The introduction of enteral nutrition increases the production of content that flows out of the ileostomy and requires the protection of the skin with a stoma bag. For this purpose, bags with circular base plates are used, which can release the contents at the bottom. However, if greater convex- ity is required due to the indentation of the scars, the protective base plate can be cut to the desired size. The bags are not changed for at least 24 to 72 hours to preserve the integrity of the skin (29). Bags point- ing downwards can become soiled with urine and can negatively affect the integrity of the skin and the

Figure 10. Healing of the surgical wound - twin V.T.
Source: Author
adhesion of the plate. If the base plate and the bag are well attached and there are no signs of leakage, the bag can be opened from the bottom and the con- tents can be removed using a syringe and the bag can be rinsed to remove the unpleasant smell. During the change of the base plate and the stoma bag, the nurse will wipe the skin around the entrance of the stoma with sterile water and slightly soft gauze, as- sess the appearance of the stoma, dry the skin with dry gauze, apply a protective spray and reattach the new base plate and bag (27). Due to the transitory immaturity of the intestines, most premature infants receive parenteral nutrition in the first few weeks of life. However, providing sufficient protein and energy to maintain optimal growth in such infants remains a challenge. Due to the immaturity of the gut during the first postnatal weeks, gastrointestinal feeding is insufficient to cover such needs at first. Despite the faster daily increase in rations, full enteral nutrition was achieved only around day 22 of life in a cohort of
preterm infants weighing less than 1000 g. Parenter- al nutrition supplies preterm infants with nutrients, but it is far from approaching the complex composi- tion of cord blood (e.g., in terms of lactate, growth factors) and should not necessarily mimic fetal nu- trient supply, dramatic changes in metabolism that occur after birth. The use of parenteral nutrition can cause serious complications (e.g., sepsis, cholestasis, thrombosis) and often does not meet the needs of premature infants (30). Therefore, it is necessary to switch to enteral nutrition as soon as possible, which in the case of these twins was difficult due to sepa- ration surgery and incomplete intestines. During the administration of breast milk through a nasogastric tube, nurses continuously assessed the appearance and behaviour of both twins, measured the circumfer- ence of the abdomen, checked the gastric retention before each feeding and checked the appearance of the stool. The course of the first twin’s stay was marked by recurrent ileus, peritonitis and difficult

Figure 11. Transfer to the Neonatal Post-Intensive Care Unit
Source: Author

Figure 12. Parents with the twins at the Neonatal Post-Intensive Care Unit
Source: Author

Figure 13. Discharge from hospital
Source: Author
healing of the surgical wound. After the first opera- tion, she initially tolerated food properly and expelled stool on the ileostomy, however, four operations were performed to treat the ileus. Peritonitis was manifested by elevated levels of inflammatory pa- rameters, a distended and painful abdomen and food intolerance. The surgical wound was difficult to heal, which required the nurse to implement interventions to prevent infection and improve healing. The nurse, with instructions from the surgeon, cleaned the sur- gical wound every day by using an aseptic method, washing the wound with a sterile saline solution, covering the surface with an Aquacell dressing to improve wound healing, and placing sterile dry dress- ings on the outer part, which she fixed with adhesive tape. It is important to note that in such cases it was also necessary to assess the surrounding skin, which was exposed to the daily change of adhesive tapes, which increased the risk of additional damage to the
integrity of the abdominal skin. The nurse assessed the appearance of the wound daily and recorded all changes in the nursing documentation in order to adequately monitor the progress of wound healing (Figure 10). Intestinal continuity was restored after 2 months, and the final closure of the abdominal wall after 4 months.
After 3 and a half months in the Neonatal Intensive Care Unit, the twins were transferred to the Neona- tal Post-Intensive Care Unit, where enteral nutrition, parental education and health care continued (Figure 11).
The birth of conjoined twins can lead to psychosocial stressors, religious dilemmas and relationships with the community. This can lead to serious disruptions in family dynamics, interactions between the medical
team and the family, and among the medical team it- self. Nurses play an extremely important role in edu- cating and supporting the parents since they spend 4 hours a day with them and through long-term hos- pitalization can assess all fears, doubts and needs of parents. The parents of the conjoined twins V. and
K. T. have been involved in the care of their children from the beginning and, with the help of nurses, es- tablished an emotional and physical bond with them. They carried out the twins’ hygiene every day, espe- cially after the separation and monitored the feed- ing of the children. The mother expressed and stored breast milk regularly so that it could be given to the twins (Figure 12). The parents were educated about the possible food intolerance and the recognition of symptoms, about the independent implementation of personal hygiene, and they were also offered the support of a priest.
During hospitalization, parents actively participated in all the interventions related to the provision of nursing care. Due to their poor financial situation, help was organized for them with clothes and equip- ment for girls, as well as housing equipment. After a little more than seven months, on August 29, 2019, the girls were discharged with recommendations for further monitoring of growth and development (Fig- ure 13).
Through coordinated care, the multidisciplinary team proactively identified the potential challenges of car- ing for conjoined twins. Nursing interventions made it possible to improve the condition and support the parents, who left the hospital extremely satisfied and still come to the Department every time the twins are scheduled for their follow-up appointment.
![]()
![]()
Conjoined twins, also known as “Siamese twins”, are a unique type of monozygotic twins and constitute an extremely rare condition that is often incompat- ible with life. However, there are types of conjoined twins in which both twins cannot be separated and survive. Continuity of care for conjoined twins re- quires the collaboration of a large number of health professionals who must work together to plan inter-
ventions and respond to the unique challenges they face. Coordination of this care should be seamless and requires regular meetings of a multidisciplinary team that provides an effective approach to coordi- nate interventions and address all the unique chal- lenges faced in the care of conjoined twins. Nurses caring for conjoined twins must demonstrate au- tonomy, ingenuity, and passion in promoting optimal outcomes for these rare and complex patients. The paper presents the case of conjoined twins, the girls
V. and K. who were admitted to the Department of Neonatology and Intensive Care Medicine after be- ing born in the Sveti Duh Hospital. After a multidis- ciplinary assessment and diagnosis, it was decided to carry out the separation procedure. The procedure lasted 15 hours and was without complications. Car- ing for conjoined twins requires the implementation of specific nursing care procedures that are an es- sential part of care and treatment. It is extremely im- portant to know the characteristics and symptoms of this specific and extremely rare group of patients in order to be able to plan and implement specific inter- ventions. Likewise, it is important to include parents in care as well.
![]()
![]()
Kobylarz K. History of treatment of conjoined twins. Anaesthesiol Intensive Ther. 2014;46(2):116-23.
Boer LL, Schepens-Franke AN, Oostra RJ. Two is a crowd: two is a crowd: on the enigmatic etiopathogenesis of conjoined twinning. Clin Anat. 2019;32(5):722-41.
De Ugarte DA, Boechat MI, Shaw WW, Laks H, Williams H, Atkinson JB. Parasitic omphalopagus complicated by omphalocele and congenital heart disease. J Pedia- tr Surg. 2002;37(9):1357-8.
Kattel P. Conjoined Twins. JNMA J Nepal Med Assoc. 2018;56(211):708-10.
Luton A, Estrada N, Barrientez K, McGinnis J, Pitlik J, Carter A, et al. Nursing considerations and interdis- ciplinary coordination in the care of conjoined twins. Semin Perinatol. 2018;42(6):340-49.
Mutchinick OM, Luna-Muñoz L, Amar E, Bakker MK, Cle- menti M, Cocchi G, et al. Conjoined twins: a worldwide collaborative epidemiological study of the Interna- tional Clearinghouse for Birth Defects Surveillance and Research. Am J Med Genet C Semin Med Genet. 2011;157C(4):274-87.
Parmekar S, McMullen L, Washington C, Arnold JL. Role of simulation in preparation for the care of conjoined twins-prenatal preparation to separation. Semin Peri- natol. 2018;42(6):329-39.
Mian A, Gabra NI, Sharma T, Topale N, Gielecki J, Tubbs RS, et al. Conjoined twins: From conception to separa- tion, a review. Clin Anat. 2017;30(3):385-96.
Kennedy GE. The 3,000-year history of conjoined twins. West J Med. 2021;175(6):176-77.
Kokcu A, Cetinkaya MB, Aydin O, Tosun M. Conjoined twins: historical perspective and report of a case. J Ma- tern Fetal Neonatal Med. 2007;20(4):349-56.
Sliwa L, Macura B. The embryology of Siamese twins
– what we know about their mechanisms of deve- lopment today? Gin Pol Med Project. 2015;3(37):28- 32.
Kaufman MH. The embryology of conjoined twins. Childs Nerv Syst. 2004;20(8-9):508-25.
Spencer R. Parasitic conjoined twins: external, inter- nal (fetuses in fetu and teratomas), and detached (acardiacs). Clin Anat. 2001;14(6):428-44.
Spitz L. Conjoined twins. Prenat Diagn. 2005;25(9):814-9.
Hervey GR. Conjoined twins. J R Soc Med. 2005;98(6):295-6.
Frawley G. Conjoined twins in 2020 - state of the art and future directions. Curr Opin Anaesthesiol. 2020;33(3):381-7.
Separation of conjoined twins and the principle of do- uble effect. Christ Bioeth. 2006;12(3):291-300.
Kingston CA, McHugh K, Kumaradevan J, Kiely EM, Spitz L. Imaging in the preoperative assessment of co- njoined twins. Radiographics. 2001;21(5):1187-208.
Randi F, Palma P, Ponzo V, Brunetti C, Bagolan P, Marras CE. Management of intraoperative neuromoni- toring in pygopagus conjoined twins. J Neurosurg Sci. 2021;65(3):380-1.
Savulescu J, Persson I. Conjoined twins: philosophi- cal problems and ethical challenges. J Med Philos. 2016;41(1):41-55.
Faulkner J. Conjoined twins: the ethics of separation. RCM Midwives. 2006;9(3):86-7.
Johann DA, De Lazzari LS, Pedrolo E, Mingorance P, de Almeida TQ, Danski MT. Cuidados com cateter central de inserção periférica no neonato: revisão integrativa da literatura [Peripherally inserted central catheter care in neonates: an integrative literature review]. Rev Esc Enferm USP. 2012;46(6):1503-11. Portugue- se.
Mitrović Z, Komljenović I, Jakšić O, Prka Ž, Šestan Cr- nek S, Ajduković Stojsavljević R, et al. Upotreba peri- ferno uvedenoga centralnog venskog katetera (PICC) u bolesnika sa zloćudnim hematološkim bolestima
– prikaz vlastitih iskustava. Lijec Vjesn. 2014;136(5- 6). Croatian.
Raut MS, Joshi S, Maheshwari A. Stuck suction cathe- ter in endotracheal tube. Indian J Crit Care Med. 2015;19(2):113-5.
Pinto HJ, D’silva F, Sanil TS. Knowledge and practices of endotracheal suctioning amongst nursing profe- ssionals: a systematic review. Indian J Crit Care Med. 2020;24(1):23-32.
Haut C. Pediatric noninvasive ventilation. J Pediatr In- tensive Care. 2015 Jun;4(2):121-7.
Waller M. Paediatric stoma care nursing in the UK and Ireland. Br J Nurs. 2008;17(17):S25-9.
Bohr C. Best practice in stoma care for neonates and children. Nurs. Child. Young People.2018;31(5):12-3.
Mrzljak V, Plužarić J, Žarković G, Ban D, Švarc S. Smjer- nice za postupke u zdravstvenoj njezi bolesnika u kući. Hrvatska komora medicinskih sestara, Udruga medicinskih sestara zdravstvene njege u kući; 2018. Croatian.
Darmaun D, Lapillonne A, Simeoni U, Picaud JC, Rozé JC, Saliba E,et al; Committee on Nutrition of the French Society of Pediatrics (CNSFP), and French So- ciety of Neonatology (SFN). Parenteral nutrition for preterm infants: Issues and strategy. Arch Pediatr. 2018;25(4):286-94.
![]()
![]()
![]()
![]()
Sijamski blizanci jedna su od najrjeđih prirođenih anomalija s incidencijom u zapadnom svijetu od oko 1,47 na 100 000 poroda. Ovaj rijedak prirodni fenomen zastupljen je u svega 1 % monozigotnih blizanaca, tj. 0,05 % živorođenih blizanaca. Većina ih je mrtvorođena (40 do 60 %) ili umire rano u životu. Većina živorođenih ženskog je spola (75 %), zbog čega se smatra da ženski kariotip nosi korist u smislu preživljenja. Sijamski blizanci nastaju kada se zigota počinje razdvajati nakon 13. dana od oplodnje, u vremenu kada je već formiran tzv. embrionalni disk. Umjesto da nastanu dva odvojena embrija, ovo kasno razdvajanje uzrokuje nepotpuno odvajanje embrija. Naziv sijamski blizanci dolazi od sijamske braće Chan- ga i Enga Bunkera, koji su rođeni u Sijamu. Kirurško razdvajanje sijamskih blizanaca najčešće je vrlo zahtjevan i složen postupak, a često nije ni moguć. Preživljenje nakon razdvajanja ovisi o vrsti i načinu spojenosti. U radu se prikazuju sijamske blizanke koje su rođene u 33. tjednu trudnoće. U 11. tjednu trudnoće postavljena je sumnja na ventralno spa- janje blizanki (omphalopagus – spajanje u području abdomena). Dijagnoza je potvrđena fetalnom mag- netskom rezonancijom u 21. tjednu trudnoće. U dobi od 45 dana života i pri zajedničkoj tjelesnoj masi od 4700 g indicirano je njihovo razdvajanje. Dugi tijek poslijeoperacijskog oporavka i liječenja trajao je tri mjeseca i komplicirao se infekcijama i problemima cijeljenja operativne rane druge blizanke. Liječenje i oporavak zahtijevali su multidisciplinarni pristup i do- bro educirani tim liječnika i medicinskih sestara.
![]()
![]()